SCI Publications
2024


C.C. Berggren, D. Jiang, Y.F. Wang, J.A. Bergquist, L. Rupp, Z. Liu, R.S. MacLeod, A. Narayan, L. Timmins.
“Influence of Material Parameter Variability on the Predicted Coronary Artery Biomechanical Environment via Uncertainty Quantification,” Subtitled “arXiv preprint arXiv:2401.15047,” 2024.
Central to the clinical adoption of patient-specific modeling strategies is demonstrating that simulation results are reliable and safe. Indeed, simulation frameworks must be robust to uncertainty in model input(s), and levels of confidence should accompany results. In this study, we applied a coupled uncertainty quantification-finite element (FE) framework to understand the impact of uncertainty in vascular material properties on variability in predicted stresses. Univariate probability distributions were fit to material parameters derived from layer-specific mechanical behavior testing of human coronary tissue. Parameters were assumed to be probabilistically independent, allowing for efficient parameter ensemble sampling. In an idealized coronary artery geometry, a forward FE model for each parameter ensemble was created to predict tissue stresses under physiologic loading. An emulator was constructed within the UncertainSCI software using polynomial chaos techniques, and statistics and sensitivities were directly computed. Results demonstrated that material parameter uncertainty propagates to variability in predicted stresses across the vessel wall, with the largest dispersions in stress within the adventitial layer. Variability in stress was most sensitive to uncertainties in the anisotropic component of the strain energy function. Moreover, unary and binary interactions within the adventitial layer were the main contributors to stress variance, and the leading factor in stress variability was uncertainty in the stress-like material parameter that describes the contribution of the embedded fibers to the overall artery stiffness. Results from a patient-specific coronary model confirmed many of these findings. Collectively, these data highlight the impact of material property variation on uncertainty in predicted artery stresses and present a pipeline to explore and characterize forward model uncertainty in computational biomechanics.

J. Dong, E. Kwan, J.A. Bergquist, B.A. Steinberg, D.J. Dosdall, E. DiBella, R.S. MacLeod, T.J. Bunch, R. Ranjan.
“Ablation-induced left atrial mechanical dysfunction recovers in weeks after ablation,” In Journal of Interventional Cardiac Electrophysiology, Springer, 2024.
Background
The immediate impact of catheter ablation on left atrial mechanical function and the timeline for its recovery in patients undergoing ablation for atrial fibrillation (AF) remain uncertain. The mechanical function response to catheter ablation in patients with different AF types is poorly understood.
Methods
A total of 113 AF patients were included in this retrospective study. Each patient had three magnetic resonance imaging (MRI) studies in sinus rhythm: one pre-ablation, one immediate post-ablation (within 2 days after ablation), and one post-ablation follow-up MRI (≤ 3 months). We used feature tracking in the MRI cine images to determine peak longitudinal atrial strain (PLAS). We evaluated the change in strain from pre-ablation, immediately after ablation to post-ablation follow-up in a short-term study (< 50 days) and a 3-month study (3 months after ablation).
Results
The PLAS exhibited a notable reduction immediately after ablation, compared to both pre-ablation levels and those observed in follow-up studies conducted at short-term (11.1 ± 9.0 days) and 3-month (69.6 ± 39.6 days) intervals. However, there was no difference between follow-up and pre-ablation PLAS. The PLAS returned to 95% pre-ablation level within 10 days. Paroxysmal AF patients had significantly higher pre-ablation PLAS than persistent AF patients in pre-ablation MRIs. Both type AF patients had significantly lower immediate post-ablation PLAS compared with pre-ablation and post-ablation PLAS.
Conclusion
The present study suggested a significant drop in PLAS immediately after ablation. Left atrial mechanical function recovered within 10 days after ablation. The drop in PLAS did not show a substantial difference between paroxysmal and persistent AF patients.
2023


R. Kamali, E. Kwan, M. Regouski, T.J. Bunch, D.J. Dosdall, E. Hsu, R. S. Macleod, I. Polejaeva, R. Ranjan.
“Contribution of atrial myofiber architecture to atrial fibrillation,” In PLOS ONE, Vol. 18, No. 1, Public Library of Science, pp. 1--16. Jan, 2023.
DOI: 10.1371/journal.pone.0279974
Background
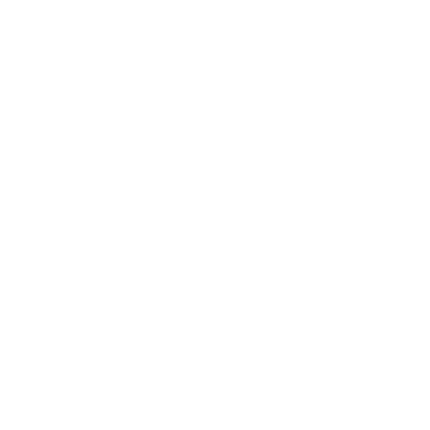
The role of fiber orientation on a global chamber level in sustaining atrial fibrillation (AF) is unknown. The goal of this study was to correlate the fiber direction derived from Diffusion Tensor Imaging (DTI) with AF inducibility.
Transgenic goats with cardiac-specific overexpression of constitutively active TGF-β1 (n = 14) underwent AF inducibility testing by rapid pacing in the left atrium. We chose a minimum of 10 minutes of sustained AF as a cut-off for AF inducibility. Explanted hearts underwent DTI to determine the fiber direction. Using tractography data, we clustered, visualized, and quantified the fiber helix angles in 8 different regions of the left atrial wall using two reference vectors defined based on anatomical landmarks.
Sustained AF was induced in 7 out of 14 goats. The mean helix fiber angles in 7 out of 8 selected regions were statistically different (P-Value < 0.05) in the AF inducible group. The average fractional anisotropy (FA) and the mean diffusivity (MD) were similar in the two groups with FA of 0.32±0.08 and MD of 8.54±1.72 mm2/s in the non-inducible group and FA of 0.31±0.05 (P-value = 0.90) and MD of 8.68±1.60 mm2/s (P-value = 0.88) in the inducible group.
DTI based fiber direction shows significant variability across subjects with a significant difference between animals that are AF inducible versus animals that are not inducible. Fiber direction might be contributing to the initiation and sustaining of AF, and its role needs to be investigated further.
2022


J. A. Bergquist, J. Coll-Font, B. Zenger, L. C. Rupp, W. W. Good, D. H. Brooks, R. S. MacLeod.
“Reconstruction of cardiac position using body surface potentials,” In Computers in Biology and Medicine, Vol. 142, pp. 105174. 2022.
DOI: https://doi.org/10.1016/j.compbiomed.2021.105174
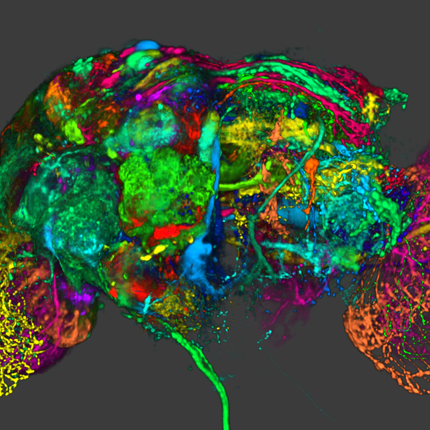
Electrocardiographic imaging (ECGI) is a noninvasive technique to assess the bioelectric activity of the heart which has been applied to aid in clinical diagnosis and management of cardiac dysfunction. ECGI is built on mathematical models that take into account several patient specific factors including the position of the heart within the torso. Errors in the localization of the heart within the torso, as might arise due to natural changes in heart position from respiration or changes in body position, contribute to errors in ECGI reconstructions of the cardiac activity, thereby reducing the clinical utility of ECGI. In this study we present a novel method for the reconstruction of cardiac geometry utilizing noninvasively acquired body surface potential measurements. Our geometric correction method simultaneously estimates the cardiac position over a series of heartbeats by leveraging an iterative approach which alternates between estimating the cardiac bioelectric source across all heartbeats and then estimating cardiac positions for each heartbeat. We demonstrate that our geometric correction method is able to reduce geometric error and improve ECGI accuracy in a wide range of testing scenarios. We examine the performance of our geometric correction method using different activation sequences, ranges of cardiac motion, and body surface electrode configurations. We find that after geometric correction resulting ECGI solution accuracy is improved and variability of the ECGI solutions between heartbeats is substantially reduced.


J.A. Bergquist, L.C. Rupp, A. Busatto, B. Orkild, B. Zenger, W. Good, J. Coll-Font, A. Narayan, J. Tate, D. Brooks, R.S. MacLeod.
“Heart Position Uncertainty Quantification in the Inverse Problem of ECGI,” In Computing in Cardiology, Vol. 49, 2022.
Electrocardiographic imaging (ECGI) is a clinical and research tool for noninvasive diagnosis of cardiac electrical dysfunction. The position of the heart within the torso is both an input and common source of error in ECGI. Many studies have sought to improve cardiac localization accuracy, however, few have examined quantitatively the effects of uncertainty in the position of the heart within the torso. Recently developed uncertainty quantification (UQ) tools enable the robust application of UQ to ECGI reconstructions. In this study, we developed an ECGI formulation, which for the first time, directly incorporated uncertainty in the heart position. The result is an ECGI solution that is robust to variation in heart position. Using data from two Langendorff experimental preparations, each with 120 heartbeats distributed across three activation sequences, we found that as heart position uncertainty increased above ±10 mm, the solution quality of the ECGI degraded. However, even at large heart position uncertainty (±40 mm) our novel UQ-ECGI formulation produced reasonable solutions (root mean squared error < 1 mV, spatial correlation >0.6, temporal correlation >0.75).


A. Busatto, J.A. Bergquist, L.C. Rupp, B. Zenger, R.S. MacLeod.
“Unexpected Errors in the Electrocardiographic Forward Problem,” In Computing in Cardiology, Vol. 49, 2022.
Previous studies have compared recorded torso potentials with electrocardiographic forward solutions from a pericardial cage. In this study, we introduce new comparisons of the forward solutions from the sock and cage with each other and with respect to the measured potentials on the torso. The forward problem of electrocardiographic imaging is expected to achieve high levels of accuracy since it is mathematically well posed. However, unexpectedly high residual errors remain between the computed and measured torso signals in experiments. A possible source of these errors is the limited spatial coverage of the cardiac sources in most experiments; most capture potentials only from the ventricles. To resolve the relationship between spatial coverage and the accuracy of the forward simulations, we combined two methods of capturing cardiac potentials using a 240-electrode sock and a 256-electrode cage, both surrounding a heart suspended in a 192-electrode torso tank. We analyzed beats from three pacing sites and calculated the RMSE, spatial correlation, and temporal correlation. We found that the forward solutions using the sock as the cardiac source were poorer compared to those obtained from the cage. In this study, we explore the differences in forward solution accuracy using the sock and the cage and suggest some possible explanations for these differences.

Y. Ishidoya, E. Kwan, D. J. Dosdall, R. S. Macleod, L. Navaravong, B. A. Steinberg, T. J. Bunch, R. Ranjan.
“Short-Term Natural Course of Esophageal Thermal Injury After Ablation for Atrial Fibrillation,” In Journal of Cardiovascular Electrophysiology, Wiley, 2022.
DOI: 10.1111/jce.15553
Purpose
To provide insight into the short-term natural history of esophageal thermal injury (ETI) after radiofrequency catheter ablation (RFCA) for atrial fibrillation (AF) by esophagogastroduodenoscopy (EGD).

Y. Ishidoya, E. Kwan, D. J. Dosdall, R. S. Macleod, L. Navaravong, B. A. Steinberg, T. J. Bunch, R. Ranjan.
“Shorter Distance Between The Esophagus And The Left Atrium Is Associated With Higher Rates Of Esophageal Thermal Injury After Radiofrequency Ablation,” In Journal of Cardiovascular Electrophysiology, Wiley, 2022.
DOI: 10.1111/jce.15554
Background
Esophageal thermal injury (ETI) is a known and potentially serious complication of catheter ablation for atrial fibrillation. We intended to evaluate the distance between the esophagus and the left atrium posterior wall (LAPW) and its association with esophageal thermal injury.

X. Jiang, Z. Li, R. Missel, Md. Zaman, B. Zenger, W. W. Good, R. S. MacLeod, J. L. Sapp, L. Wang.
“Few-Shot Generation of Personalized Neural Surrogates for Cardiac Simulation via Bayesian Meta-learning,” In Medical Image Computing and Computer Assisted Intervention -- MICCAI 2022, Springer Nature Switzerland, pp. 46--56. 2022.
ISBN: 978-3-031-16452-1
DOI: 10.1007/978-3-031-16452-1_5
Clinical adoption of personalized virtual heart simulations faces challenges in model personalization and expensive computation. While an ideal solution is an efficient neural surrogate that at the same time is personalized to an individual subject, the state-of-the-art is either concerned with personalizing an expensive simulation model, or learning an efficient yet generic surrogate. This paper presents a completely new concept to achieve personalized neural surrogates in a single coherent framework of meta-learning (metaPNS). Instead of learning a single neural surrogate, we pursue the process of learning a personalized neural surrogate using a small amount of context data from a subject, in a novel formulation of few-shot generative modeling underpinned by: 1) a set-conditioned neural surrogate for cardiac simulation that, conditioned on subject-specific context data, learns to generate query simulations not included in the context set, and 2) a meta-model of amortized variational inference that learns to condition the neural surrogate via simple feed-forward embedding of context data. As test time, metaPNS delivers a personalized neural surrogate by fast feed-forward embedding of a small and flexible number of data available from an individual, achieving -- for the first time -- personalization and surrogate construction for expensive simulations in one end-to-end learning framework. Synthetic and real-data experiments demonstrated that metaPNS was able to improve personalization and predictive accuracy in comparison to conventionally-optimized cardiac simulation models, at a fraction of computation.


X. Jiang, M. Toloubidokhti, J. Bergquist, B. Zenger, w. Good, R.S. MacLeod, L. Wang.
“Improving Generalization by Learning Geometry-Dependent and Physics-Based Reconstruction of Image Sequences,” In IEEE Transactions on Medical Imaging, 2022.
DOI: 10.1109/TMI.2022.3218170
Deep neural networks have shown promise in image reconstruction tasks, although often on the premise of large amounts of training data. In this paper, we present a new approach to exploit the geometry and physics underlying electrocardiographic imaging (ECGI) to learn efficiently with a relatively small dataset. We first introduce a non-Euclidean encoding-decoding network that allows us to describe the unknown and measurement variables over their respective geometrical domains. We then explicitly model the geometry-dependent physics in between the two domains via a bipartite graph over their graphical embeddings. We applied the resulting network to reconstruct electrical activity on the heart surface from body-surface potentials. In a series of generalization tasks with increasing difficulty, we demonstrated the improved ability of the network to generalize across geometrical changes underlying the data using less than 10% of training data and fewer variations of training geometry in comparison to its Euclidean alternatives. In both simulation and real-data experiments, we further demonstrated its ability to be quickly fine-tuned to new geometry using a modest amount of data.


R. Kamali, K. Gillete, J. Tate, D. A. Abhyankar, D. J. Dosdall, G. Plank, T. J. Bunch, R. S. Macleod & R. Ranjan .
“Treatment Planning for Atrial Fibrillation Using Patient-Specific Models Showing the Importance of Fibrillatory-Areas,” In Annals of Biomedical Engineering, Springer, 2022.
DOI: https://doi.org/10.1007/s10439-022-03029-5
Computational models have made it possible to study the effect of fibrosis and scar on atrial fibrillation (AF) and plan future personalized treatments. Here, we study the effect of area available for fibrillatory waves to sustain AF. Then we use it to plan for AF ablation to improve procedural outcomes. CARPentry was used to create patient-specific models to determine the association between the size of residual contiguous areas available for AF wavefronts to propagate and sustain AF [fibrillatory area (FA)] after ablation with procedural outcomes. The FA was quantified in a novel manner accounting for gaps in ablation lines. We selected 30 persistent AF patients with known ablation outcomes. We divided the atrial surface into five areas based on ablation scar pattern and anatomical landmarks and calculated the FAs. We validated the models based on clinical outcomes and suggested future ablation lines that minimize the FAs and terminate rotor activities in simulations. We also simulated the effects of three common antiarrhythmic drugs. In the patient-specific models, the predicted arrhythmias matched the clinical outcomes in 25 of 30 patients (accuracy 83.33%). The average largest FA (FAmax) in the recurrence group was 8517 ± 1444 vs. 6772 ± 1531 mm2 in the no recurrence group (p < 0.004). The final FAs after adding the suggested ablation lines in the AF recurrence group reduced the average FAmax from 8517 ± 1444 to 6168 ± 1358 mm2 (p < 0.001) and stopped the sustained rotor activity. Simulations also correctly anticipated the effect of antiarrhythmic drugs in 5 out of 6 patients who used drug therapy post unsuccessful ablation (accuracy 83.33%). Sizes of FAs available for AF wavefronts to propagate are important determinants for ablation outcomes. FA size in combination with computational simulations can be used to direct ablation in persistent AF to minimize the critical mass required to sustain recurrent AF.


A. Narayan, Z. Liu, J. A. Bergquist, C. Charlebois, S. Rampersad, L. Rupp, D. Brooks, D. White, J. Tate, R. S. MacLeod.
“UncertainSCI: Uncertainty quantification for computational models in biomedicine and bioengineering,” In Computers in Biology and Medicine, 2022.
DOI: https://doi.org/10.1016/j.compbiomed.2022.106407
Background:
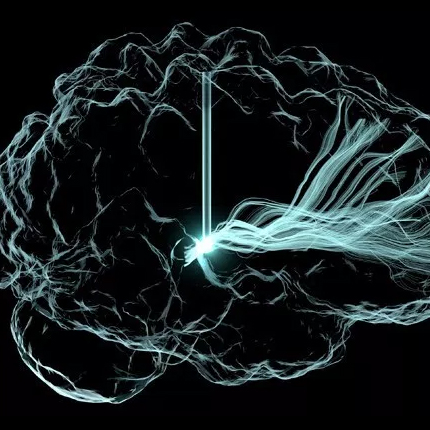
Computational biomedical simulations frequently contain parameters that model physical features, material coefficients, and physiological effects, whose values are typically assumed known a priori. Understanding the effect of variability in those assumed values is currently a topic of great interest. A general-purpose software tool that quantifies how variation in these parameters affects model outputs is not broadly available in biomedicine. For this reason, we developed the ‘UncertainSCI’ uncertainty quantification software suite to facilitate analysis of uncertainty due to parametric variability.
We developed and distributed a new open-source Python-based software tool, UncertainSCI, which employs advanced parameter sampling techniques to build polynomial chaos (PC) emulators that can be used to predict model outputs for general parameter values. Uncertainty of model outputs is studied by modeling parameters as random variables, and model output statistics and sensitivities are then easily computed from the emulator. Our approaches utilize modern, near-optimal techniques for sampling and PC construction based on weighted Fekete points constructed by subsampling from a suitably randomized candidate set.
Concentrating on two test cases—modeling bioelectric potentials in the heart and electric stimulation in the brain—we illustrate the use of UncertainSCI to estimate variability, statistics, and sensitivities associated with multiple parameters in these models.
UncertainSCI is a powerful yet lightweight tool enabling sophisticated probing of parametric variability and uncertainty in biomedical simulations. Its non-intrusive pipeline allows users to leverage existing software libraries and suites to accurately ascertain parametric uncertainty in a variety of applications.


B.A. Orkild, J.A. Bergquist, L.C. Rupp, A. Busatto, B. Zenger, W.W. Good, J. Coll-Font, R.S. MacLeod.
“A Sliding Window Approach to Regularization in Electrocardiographic Imaging,” In Computing in Cardiology, Vol. 49, 2022.
Introduction: The inverse problem of ECGI is ill-posed, so regularization must be applied to constrain the solution. Regularization is typically applied to each individual time point (instantaneous) or to the beat as a whole (global). These techniques often lead to over- or underregularization. We aimed to develop an inverse formulation that strikes a balance between these two approaches that would realize the benefits of both by implementing a sliding-window regularization. Methods: We formulated sliding-window regularization using the boundary element method with Tikhonov 0 and 2nd order regularization. We applied regularization to a varying time window of the body-surface potentials centered around each time sample. We compared reconstructed potentials from the sliding-window, instantaneous, and global regularization techniques to ground truth potentials for 10 heart beats paced from the ventricle in a large-animal model. Results: The sliding-window technique provided smoother transitions of regularization weights than instantaneous regularization while improving spatial correlation over global regularization. Discussion: Although the differences in regularization weights were nuanced, smoother transitions provided by the sliding-window regularization have the ability to eliminate discontinuities in potential seen with instantaneous regularization.


L.C. Rupp, B. Zenger, J.A. Bergquist, A. Busatto, R.S. MacLeod.
“The Role of Beta-1 Receptors in the Response to Myocardial Ischemia,” In Computing in Cardiology, Vol. 49, 2022.
Acute myocardial ischemia is commonly diagnosed by ST-segment deviations. These deviations, however, can show a paradoxical recovery even in the face of ongoing ischemic stress. A possible mechanism for this response may be the cardio-protective effects of the autonomic nervous system (ANS) via beta-1 receptors. We assessed the role of norepinephrine (NE), a beta-1 agonist, and esmolol (ES), a beta-1 antagonist, in the recovery of ST-segment deviations during myocardial ischemia. We used an experimental model of controlled myocardial ischemia in which we simultaneously recorded electrograms intramurally and on the epicardial surface. We measured ischemia as deviations in the potentials measured at 40% of the ST-segment duration. During control intervention, 27% of epicardial electrodes showed no ischemic ST-segment deviations, whereas during the interventions with NE and ES, 100% of epicardial electrodes showed no ischemic ST-segment deviations. Intramural electrodes revealed a different behavior with 71% of electrodes showing no ischemic ST-segment deviations during control ischemia, increasing to 79% and 82% for NE infusion and ES infusion interventions, respectively. These preliminary results suggest that recovery of intramural regions of the heart is delayed by the presence of both beta-1 agonists and antagonists even as epicardial potentials show almost complete recovery.

M. Toloubidokhti, N. Kumar, Z. Li, P. K. Gyawali, B. Zenger, W. W. Good, R. S. MacLeod, L. Wang .
“Interpretable Modeling and Reduction of Unknown Errors in Mechanistic Operators,” In Medical Image Computing and Computer Assisted Intervention -- MICCAI 2022, Springer Nature Switzerland, pp. 459--468. 2022.
ISBN: 978-3-031-16452-1
DOI: 10.1007/978-3-031-16452-1_44
Prior knowledge about the imaging physics provides a mechanistic forward operator that plays an important role in image reconstruction, although myriad sources of possible errors in the operator could negatively impact the reconstruction solutions. In this work, we propose to embed the traditional mechanistic forward operator inside a neural function, and focus on modeling and correcting its unknown errors in an interpretable manner. This is achieved by a conditional generative model that transforms a given mechanistic operator with unknown errors, arising from a latent space of self-organizing clusters of potential sources of error generation. Once learned, the generative model can be used in place of a fixed forward operator in any traditional optimization-based reconstruction process where, together with the inverse solution, the error in prior mechanistic forward operator can be minimized and the potential source of error uncovered. We apply the presented method to the reconstruction of heart electrical potential from body surface potential. In controlled simulation experiments and in-vivo real data experiments, we demonstrate that the presented method allowed reduction of errors in the physics-based forward operator and thereby delivered inverse reconstruction of heart-surface potential with increased accuracy.
2021


J. A. Bergquist, W. W. Good, B. Zenger, J. D. Tate, L. C. Rupp, R. S. MacLeod.
“The Electrocardiographic Forward Problem: A Benchmark Study,” In Computers in Biology and Medicine, Vol. 134, Pergamon, pp. 104476. 2021.
DOI: https://doi.org/10.1016/j.compbiomed.2021.104476
Background
Electrocardiographic forward problems are crucial components for noninvasive electrocardiographic imaging (ECGI) that compute torso potentials from cardiac source measurements. Forward problems have few sources of error as they are physically well posed and supported by mature numerical and computational techniques. However, the residual errors reported from experimental validation studies between forward computed and measured torso signals remain surprisingly high.
Objective
To test the hypothesis that incomplete cardiac source sampling, especially above the atrioventricular (AV) plane is a major contributor to forward solution errors.
Methods
We used a modified Langendorff preparation suspended in a human-shaped electrolytic torso-tank and a novel pericardiac-cage recording array to thoroughly sample the cardiac potentials. With this carefully controlled experimental preparation, we minimized possible sources of error, including geometric error and torso inhomogeneities. We progressively removed recorded signals from above the atrioventricular plane to determine how the forward-computed torso-tank potentials were affected by incomplete source sampling.
Results
We studied 240 beats total recorded from three different activation sequence types (sinus, and posterior and anterior left-ventricular free-wall pacing) in each of two experiments. With complete sampling by the cage electrodes, all correlation metrics between computed and measured torso-tank potentials were above 0.93 (maximum 0.99). The mean root-mean-squared error across all beat types was also low, less than or equal to 0.10 mV. A precipitous drop in forward solution accuracy was observed when we included only cage measurements below the AV plane.
Conclusion
First, our forward computed potentials using complete cardiac source measurements set a benchmark for similar studies. Second, this study validates the importance of complete cardiac source sampling above the AV plane to produce accurate forward computed torso potentials. Testing ECGI systems and techniques with these more complete and highly accurate datasets will improve inverse techniques and noninvasive detection of cardiac electrical abnormalities.


W. W. Good, B. Zenger, J. A. Bergquist, L. C. Rupp, K. K. Gillette, M. A.F. Gsell, G. Plank, R. S. MacLeod.
“Quantifying the spatiotemporal influence of acute myocardial ischemia on volumetric conduction velocity,” In Journal of Electrocardiology, Vol. 66, Churchill Livingstone, pp. 86-94. 2021.
Introduction
Acute myocardial ischemia occurs when coronary perfusion to the heart is inadequate, which can perturb the highly organized electrical activation of the heart and can result in adverse cardiac events including sudden cardiac death. Ischemia is known to influence the ST and repolarization phases of the ECG, but it also has a marked effect on propagation (QRS); however, studies investigating propagation during ischemia have been limited.


W. W. Good, K. Gillette, B. Zenger, J. Bergquist, L. C. Rupp, J. D. Tate, D. Anderson, M. Gsell, G. Plank, R. S. Macleod.
“Estimation and validation of cardiac conduction velocity and wavefront reconstruction using epicardial and volumetric data,” In IEEE Transactions on Biomedical Engineering, IEEE, 2021.
DOI: 10.1109/TBME.2021.3069792
Objective: In this study, we have used whole heart simulations parameterized with large animal experiments to validate three techniques (two from the literature and one novel) for estimating epicardial and volumetric conduction velocity (CV). Methods: We used an eikonal-based simulation model to generate ground truth activation sequences with prescribed CVs. Using the sampling density achieved experimentally we examined the accuracy with which we could reconstruct the wavefront, and then examined the robustness of three CV estimation techniques to reconstruction related error. We examined a triangulation-based, inverse-gradient-based, and streamline-based techniques for estimating CV cross the surface and within the volume of the heart. Results: The reconstructed activation times agreed closely with simulated values, with 50-70% of the volumetric nodes and 97-99% of the epicardial nodes were within 1 ms of the ground truth. We found close agreement between the CVs calculated using reconstructed versus ground truth activation times, with differences in the median estimated CV on the order of 3-5% volumetrically and 1-2% superficially, regardless of what technique was used. Conclusion: Our results indicate that the wavefront reconstruction and CV estimation techniques are accurate, allowing us to examine changes in propagation induced by experimental interventions such as acute ischemia, ectopic pacing, or drugs. Significance: We implemented, validated, and compared the performance of a number of CV estimation techniques. The CV estimation techniques implemented in this study produce accurate, high-resolution CV fields that can be used to study propagation in the heart experimentally and clinically.


W. W. Good, B. Zenger, J. A. Bergquist, L. C. Rupp, K. Gillett, N. Angel, D. Chou, G. Plank, R. S. MacLeod.
“Combining endocardial mapping and electrocardiographic imaging (ECGI) for improving PVC localization: A feasibility study,” In Journal of Electrocardiology, 2021.
ISSN: 0022-0736
DOI: https://doi.org/10.1016/j.jelectrocard.2021.08.013
Introduction
Accurate reconstruction of cardiac activation wavefronts is crucial for clinical diagnosis, management, and treatment of cardiac arrhythmias. Furthermore, reconstruction of activation profiles within the intramural myocardium has long been impossible because electrical mapping was only performed on the endocardial surface. Recent advancements in electrocardiographic imaging (ECGI) have made endocardial and epicardial activation mapping possible. We propose a novel approach to use both endocardial and epicardial mapping in a combined approach to reconstruct intramural activation times.
To implement and validate a combined epicardial/endocardial intramural activation time reconstruction technique.
We used 11 simulations of ventricular activation paced from sites throughout myocardial wall and extracted endocardial and epicardial activation maps at approximate clinical resolution. From these maps, we interpolated the activation times through the myocardium using thin-plate-spline radial basis functions. We evaluated activation time reconstruction accuracy using root-mean-squared error (RMSE) of activation times and the percent of nodes within 1 ms of the ground truth.
Reconstructed intramural activation times showed an RMSE and percentage of nodes within 1 ms of the ground truth simulations of 3 ms and 70%, respectively. In the worst case, the RMSE and percentage of nodes were 4 ms and 60%, respectively.
Conclusion
We showed that a simple, yet effective combination of clinical endocardial and epicardial activation maps can accurately reconstruct intramural wavefronts. Furthermore, we showed that this approach provided robust reconstructions across multiple intramural stimulation sites.

X. Jiang, J. C. Font, J. A. Bergquist, B. Zenger, W. W. Good, D. H. Brooks, R. S. MacLeod, L. Wang.
“Deep Adaptive Electrocardiographic Imaging with Generative Forward Model for Error Reduction,” In Functional Imaging and Modeling of the Heart: 11th International Conference, In Functional Imaging and Modeling of the Heart: 11th International Conference, Vol. 12738, Springer Nature, pp. 471. 2021.
Accuracy of estimating the heart’s electrical activity with Electrocardiographic Imaging (ECGI) is challenging due to using an error-prone physics-based model (forward model). While getting better results than the traditional numerical methods following the underlying physics, modern deep learning approaches ignore the physics behind the electrical propagation in the body and do not allow the use of patientspecific geometry. We introduce a deep-learning-based ECGI framework capable of understanding the underlying physics, aware of geometry, and adjustable to patient-specific data. Using a variational autoencoder (VAE), we uncover the forward model’s parameter space, and when solving the inverse problem, these parameters will be optimized to reduce the errors in the forward model. In both simulation and real data experiments, we demonstrated the ability of the presented framework to provide accurate reconstruction of the heart’s electrical potentials and localization of the earliest activation sites.