Biomedical Computing
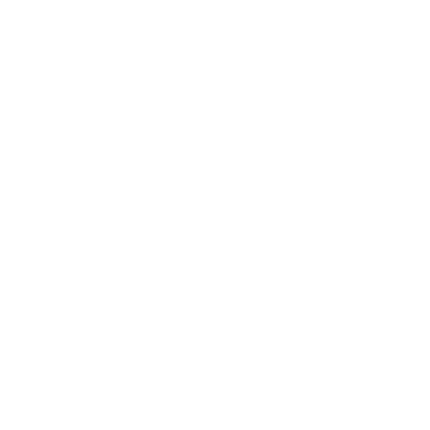
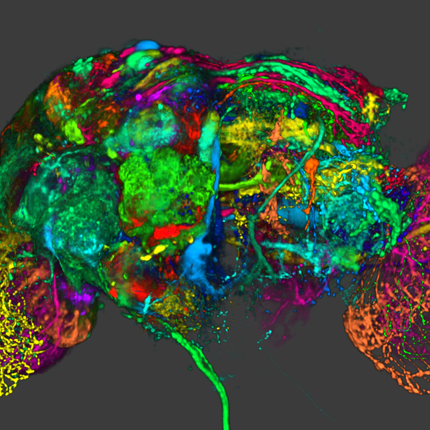
Biomedical computing combines the diagnostic and investigative aspects of biology and medical science with the power and problem-solving capabilities of modern computing. Computers are used to accelerate research learning, simulate patient behavior and visualize complex biological models.
Jeff Weiss
Computational Biomechanics
Orly Alter
Computational Biology
Tamara Bidone
Computational Models
Simulations of Biological Systems
Multi-Physics Models of Cancer Cells
Centers and Labs:
- Center for Integrative Biomedical Computing
- Muskuloskeletal Research Laboratory
- Genomic Signal Processing Lab
- Computational Biomechanics Group
Funded Research Projects:
Publications in Biomedical Computing:
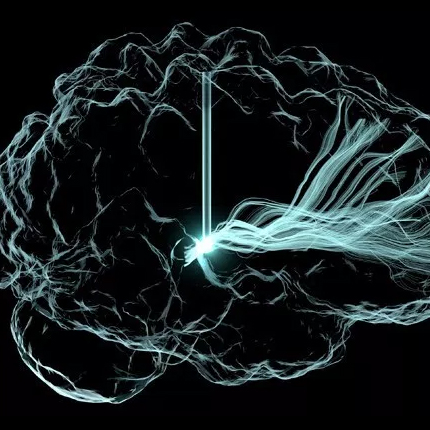
  UncertainSCI: Uncertainty quantification for computational models in biomedicine and bioengineering A. Narayan, Z. Liu, J. A. Bergquist, C. Charlebois, S. Rampersad, L. Rupp, D. Brooks, D. White, J. Tate, R. S. MacLeod. In Computers in Biology and Medicine, 2022. DOI: https://doi.org/10.1016/j.compbiomed.2022.106407 Background: Methods:
We developed and distributed a new open-source Python-based software tool, UncertainSCI, which employs advanced parameter sampling techniques to build polynomial chaos (PC) emulators that can be used to predict model outputs for general parameter values. Uncertainty of model outputs is studied by modeling parameters as random variables, and model output statistics and sensitivities are then easily computed from the emulator. Our approaches utilize modern, near-optimal techniques for sampling and PC construction based on weighted Fekete points constructed by subsampling from a suitably randomized candidate set. Results:
Concentrating on two test cases—modeling bioelectric potentials in the heart and electric stimulation in the brain—we illustrate the use of UncertainSCI to estimate variability, statistics, and sensitivities associated with multiple parameters in these models. Conclusion:
UncertainSCI is a powerful yet lightweight tool enabling sophisticated probing of parametric variability and uncertainty in biomedical simulations. Its non-intrusive pipeline allows users to leverage existing software libraries and suites to accurately ascertain parametric uncertainty in a variety of applications. |
  Comparing different nonlinear dimensionality reduction techniques for data-driven unsteady fluid flow modeling H. Csala, S.T.M. Dawson, A. Arzani. In Physics of Fluids, AIP Publishing, 2022. DOI: https://doi.org/10.1063/5.0127284 Computational fluid dynamics (CFD) is known for producing high-dimensional spatiotemporal data. Recent advances in machine learning (ML) have introduced a myriad of techniques for extracting physical information from CFD. Identifying an optimal set of coordinates for representing the data in a low-dimensional embedding is a crucial first step toward data-driven reduced-order modeling and other ML tasks. This is usually done via principal component analysis (PCA), which gives an optimal linear approximation. However, fluid flows are often complex and have nonlinear structures, which cannot be discovered or efficiently represented by PCA. Several unsupervised ML algorithms have been developed in other branches of science for nonlinear dimensionality reduction (NDR), but have not been extensively used for fluid flows. Here, four manifold learning and two deep learning (autoencoder)-based NDR methods are investigated and compared to PCA. These are tested on two canonical fluid flow problems (laminar and turbulent) and two biomedical flows in brain aneurysms. The data reconstruction capabilities of these methods are compared, and the challenges are discussed. The temporal vs spatial arrangement of data and its influence on NDR mode extraction is investigated. Finally, the modes are qualitatively compared. The results suggest that using NDR methods would be beneficial for building more efficient reduced-order models of fluid flows. All NDR techniques resulted in smaller reconstruction errors for spatial reduction. Temporal reduction was a harder task; nevertheless, it resulted in physically interpretable modes. Our work is one of the first comprehensive comparisons of various NDR methods in unsteady flows. |
  Improving Generalization by Learning Geometry-Dependent and Physics-Based Reconstruction of Image Sequences X. Jiang, M. Toloubidokhti, J. Bergquist, B. Zenger, w. Good, R.S. MacLeod, L. Wang. In IEEE Transactions on Medical Imaging, 2022. DOI: 10.1109/TMI.2022.3218170 Deep neural networks have shown promise in image reconstruction tasks, although often on the premise of large amounts of training data. In this paper, we present a new approach to exploit the geometry and physics underlying electrocardiographic imaging (ECGI) to learn efficiently with a relatively small dataset. We first introduce a non-Euclidean encoding-decoding network that allows us to describe the unknown and measurement variables over their respective geometrical domains. We then explicitly model the geometry-dependent physics in between the two domains via a bipartite graph over their graphical embeddings. We applied the resulting network to reconstruct electrical activity on the heart surface from body-surface potentials. In a series of generalization tasks with increasing difficulty, we demonstrated the improved ability of the network to generalize across geometrical changes underlying the data using less than 10% of training data and fewer variations of training geometry in comparison to its Euclidean alternatives. In both simulation and real-data experiments, we further demonstrated its ability to be quickly fine-tuned to new geometry using a modest amount of data. |
 Interpretable Modeling and Reduction of Unknown Errors in Mechanistic Operators, M. Toloubidokhti, N. Kumar, Z. Li, P. K. Gyawali, B. Zenger, W. W. Good, R. S. MacLeod, L. Wang . In Medical Image Computing and Computer Assisted Intervention -- MICCAI 2022, Springer Nature Switzerland, pp. 459--468. 2022. ISBN: 978-3-031-16452-1 DOI: 10.1007/978-3-031-16452-1_44 Prior knowledge about the imaging physics provides a mechanistic forward operator that plays an important role in image reconstruction, although myriad sources of possible errors in the operator could negatively impact the reconstruction solutions. In this work, we propose to embed the traditional mechanistic forward operator inside a neural function, and focus on modeling and correcting its unknown errors in an interpretable manner. This is achieved by a conditional generative model that transforms a given mechanistic operator with unknown errors, arising from a latent space of self-organizing clusters of potential sources of error generation. Once learned, the generative model can be used in place of a fixed forward operator in any traditional optimization-based reconstruction process where, together with the inverse solution, the error in prior mechanistic forward operator can be minimized and the potential source of error uncovered. We apply the presented method to the reconstruction of heart electrical potential from body surface potential. In controlled simulation experiments and in-vivo real data experiments, we demonstrate that the presented method allowed reduction of errors in the physics-based forward operator and thereby delivered inverse reconstruction of heart-surface potential with increased accuracy. |
 Few-Shot Generation of Personalized Neural Surrogates for Cardiac Simulation via Bayesian Meta-learning, X. Jiang, Z. Li, R. Missel, Md. Zaman, B. Zenger, W. W. Good, R. S. MacLeod, J. L. Sapp, L. Wang. In Medical Image Computing and Computer Assisted Intervention -- MICCAI 2022, Springer Nature Switzerland, pp. 46--56. 2022. ISBN: 978-3-031-16452-1 DOI: 10.1007/978-3-031-16452-1_5 Clinical adoption of personalized virtual heart simulations faces challenges in model personalization and expensive computation. While an ideal solution is an efficient neural surrogate that at the same time is personalized to an individual subject, the state-of-the-art is either concerned with personalizing an expensive simulation model, or learning an efficient yet generic surrogate. This paper presents a completely new concept to achieve personalized neural surrogates in a single coherent framework of meta-learning (metaPNS). Instead of learning a single neural surrogate, we pursue the process of learning a personalized neural surrogate using a small amount of context data from a subject, in a novel formulation of few-shot generative modeling underpinned by: 1) a set-conditioned neural surrogate for cardiac simulation that, conditioned on subject-specific context data, learns to generate query simulations not included in the context set, and 2) a meta-model of amortized variational inference that learns to condition the neural surrogate via simple feed-forward embedding of context data. As test time, metaPNS delivers a personalized neural surrogate by fast feed-forward embedding of a small and flexible number of data available from an individual, achieving -- for the first time -- personalization and surrogate construction for expensive simulations in one end-to-end learning framework. Synthetic and real-data experiments demonstrated that metaPNS was able to improve personalization and predictive accuracy in comparison to conventionally-optimized cardiac simulation models, at a fraction of computation. |
 Quantifying and Visualizing Uncertainty for Source Localisation in Electrocardiographic Imaging, D. K. Njeru, T. M. Athawale, J. J. France, C. R. Johnson. In Computer Methods in Biomechanics and Biomedical Engineering: Imaging & Visualization, Taylor & Francis, pp. 1--11. 2022. DOI: 10.1080/21681163.2022.2113824 Electrocardiographic imaging (ECGI) presents a clinical opportunity to noninvasively understand the sources of arrhythmias for individual patients. To help increase the effectiveness of ECGI, we provide new ways to visualise associated measurement and modelling errors. In this paper, we study source localisation uncertainty in two steps: First, we perform Monte Carlo simulations of a simple inverse ECGI source localisation model with error sampling to understand the variations in ECGI solutions. Second, we present multiple visualisation techniques, including confidence maps, level-sets, and topology-based visualisations, to better understand uncertainty in source localization. Our approach offers a new way to study uncertainty in the ECGI pipeline. |
  Treatment Planning for Atrial Fibrillation Using Patient-Specific Models Showing the Importance of Fibrillatory-Areas R. Kamali, K. Gillete, J. Tate, D. A. Abhyankar, D. J. Dosdall, G. Plank, T. J. Bunch, R. S. Macleod & R. Ranjan . In Annals of Biomedical Engineering, Springer, 2022. DOI: https://doi.org/10.1007/s10439-022-03029-5 Computational models have made it possible to study the effect of fibrosis and scar on atrial fibrillation (AF) and plan future personalized treatments. Here, we study the effect of area available for fibrillatory waves to sustain AF. Then we use it to plan for AF ablation to improve procedural outcomes. CARPentry was used to create patient-specific models to determine the association between the size of residual contiguous areas available for AF wavefronts to propagate and sustain AF [fibrillatory area (FA)] after ablation with procedural outcomes. The FA was quantified in a novel manner accounting for gaps in ablation lines. We selected 30 persistent AF patients with known ablation outcomes. We divided the atrial surface into five areas based on ablation scar pattern and anatomical landmarks and calculated the FAs. We validated the models based on clinical outcomes and suggested future ablation lines that minimize the FAs and terminate rotor activities in simulations. We also simulated the effects of three common antiarrhythmic drugs. In the patient-specific models, the predicted arrhythmias matched the clinical outcomes in 25 of 30 patients (accuracy 83.33%). The average largest FA (FAmax) in the recurrence group was 8517 ± 1444 vs. 6772 ± 1531 mm2 in the no recurrence group (p < 0.004). The final FAs after adding the suggested ablation lines in the AF recurrence group reduced the average FAmax from 8517 ± 1444 to 6168 ± 1358 mm2 (p < 0.001) and stopped the sustained rotor activity. Simulations also correctly anticipated the effect of antiarrhythmic drugs in 5 out of 6 patients who used drug therapy post unsuccessful ablation (accuracy 83.33%). Sizes of FAs available for AF wavefronts to propagate are important determinants for ablation outcomes. FA size in combination with computational simulations can be used to direct ablation in persistent AF to minimize the critical mass required to sustain recurrent AF. |
 Relating Metopic Craniosynostosis Severity to Intracranial Pressure, J.D. Blum, J. Beiriger, C. Kalmar, R.A. Avery, S. Lang, D.F. Villavisanis, L. Cheung, D.Y. Cho, W. Tao, R. Whitaker, S.P. Bartlett, J.A. Taylor, J.A. Goldstein, J.W. Swanson. In The Journal of Craniofacial Surgery, 2022. DOI: 10.1097/SCS.0000000000008748 Purpose: Methods:
Children with nonsyndromic single-suture metopic synostosis were prospectively enrolled and underwent optical coherence tomography to measure optic nerve head morphology. Preoperative head computed tomography scans were assessed for endocranial bifrontal angle as well as scaled metopic synostosis severity score (MSS) and cranial morphology deviation score determined by CranioRate, an automated severity classifier. Results:
Forty-seven subjects were enrolled between 2014 and 2019, at an average age of 8.5 months at preoperative computed tomography and 11.8 months at index procedure. Fourteen patients (29.7%) had elevated optical coherence tomography parameters suggestive of elevated ICP at the time of surgery. Ten patients (21.3%) had been diagnosed with developmental delay, eight of whom demonstrated elevated ICP. There were no significant associations between measures of metopic severity and ICP. Metopic synostosis severity score and endocranial bifrontal angle were inversely correlated, as expected (r=−0.545, P<0.001). A negative correlation was noted between MSS and formally diagnosed developmental delay (r=−0.387, P=0.008). Likewise, negative correlations between age at procedure and both MSS and cranial morphology deviation was observed (r=−0.573, P<0.001 and r=−0.312, P=0.025, respectively). Conclusions:
Increased metopic severity was not associated with elevated ICP at the time of surgery. Patients who underwent later surgical correction showed milder phenotypic dysmorphology with an increased incidence of developmental delay. |
 Shorter Distance Between The Esophagus And The Left Atrium Is Associated With Higher Rates Of Esophageal Thermal Injury After Radiofrequency Ablation, Y. Ishidoya, E. Kwan, D. J. Dosdall, R. S. Macleod, L. Navaravong, B. A. Steinberg, T. J. Bunch, R. Ranjan. In Journal of Cardiovascular Electrophysiology, Wiley, 2022. DOI: 10.1111/jce.15554 Background Methods
A retrospective analysis of 73 patients who underwent esophagogastroduodenoscopy (EGD) after LA radiofrequency catheter ablation for symptomatic atrial fibrillation and pre-ablation magnetic resonance imaging (MRI) was used to identify the minimum distance between the inner lumen of the esophagus and the ablated atrial endocardium (pre-ablation atrial esophageal distance; pre-AED) and occurrence of ETI. Parameters of ablation index (AI, Visitag Surpoint) were collected in 30 patients from the CARTO3 system and compared to assess if ablation strategies and AI further impacted risk of ETI.Results
Pre-AED was significantly larger in patients without ETI than those with ETI (5.23 ± 0.96 mm vs 4.31 ± 0.75 mm, p < 0.001). Pre-AED showed high accuracy for predicting ETI with the best cutoff value of 4.37 mm. AI was statistically comparable between Visitag lesion markers with and without associated esophageal late gadolinium enhancement (LGE) detected by post-ablation MRI in the low-power long-duration ablation group (LPLD, 25-40W for 10 to 30 s, 393.16 [308.62, 408.86] versus 406.58 [364.38, 451.22], p = 0.16) and high-power short-duration group (HPSD, 50W for 5-10 s, 336.14 [299.66, 380.11] versus 330.54 [286.21, 384.71], p = 0.53), respectively.Conclusion
Measuring the distance between the LA and the esophagus in pre-ablation LGE-MRI could be helpful in predicting ETI after LAPW ablation.
|
 Short-Term Natural Course of Esophageal Thermal Injury After Ablation for Atrial Fibrillation, Y. Ishidoya, E. Kwan, D. J. Dosdall, R. S. Macleod, L. Navaravong, B. A. Steinberg, T. J. Bunch, R. Ranjan. In Journal of Cardiovascular Electrophysiology, Wiley, 2022. DOI: 10.1111/jce.15553 Purpose Methods
We screened patients who underwent RFCA for AF and EGD based on esophageal late gadolinium enhancement (LGE) in post ablation MRI. Patients with ETI diagnosed with EGD were included. We defined severity of ETI according to Kansas City classification (KCC): type 1: erythema; type 2: ulcers (2a: superficial; 2b deep); type 3 perforation (3a: perforation; 3b: perforation with atrioesophageal fistula). Repeated EGD was performed within 1-14 days after the last EGD if recommended and possible until any certain healing signs (visible reduction in size without deepening of ETI or complete resolution) were observed.Results
ETI was observed in 62 of 378 patients who underwent EGD after RFCA. Out of these 62 patients with ETI, 21% (13) were type 1, 50% (31) were type 2a and 29% (18) were type 2b at the initial EGD. All esophageal lesions, but one type 2b lesion that developed into an atrioesophageal fistula (AEF), showed signs of healing in repeated EGD studies within 14 days after the procedure. The one type 2b lesion developing into an AEF showed an increase in size and ulcer deepening in repeat EGD 8 days after the procedure.Conclusion
We found that all ETI which didn't progress to AEF presented healing signs within 14 days after the procedure and that worsening ETI might be an early signal for developing esophageal perforation.
|
  Reconstruction of cardiac position using body surface potentials J. A. Bergquist, J. Coll-Font, B. Zenger, L. C. Rupp, W. W. Good, D. H. Brooks, R. S. MacLeod. In Computers in Biology and Medicine, Vol. 142, pp. 105174. 2022. DOI: https://doi.org/10.1016/j.compbiomed.2021.105174 Electrocardiographic imaging (ECGI) is a noninvasive technique to assess the bioelectric activity of the heart which has been applied to aid in clinical diagnosis and management of cardiac dysfunction. ECGI is built on mathematical models that take into account several patient specific factors including the position of the heart within the torso. Errors in the localization of the heart within the torso, as might arise due to natural changes in heart position from respiration or changes in body position, contribute to errors in ECGI reconstructions of the cardiac activity, thereby reducing the clinical utility of ECGI. In this study we present a novel method for the reconstruction of cardiac geometry utilizing noninvasively acquired body surface potential measurements. Our geometric correction method simultaneously estimates the cardiac position over a series of heartbeats by leveraging an iterative approach which alternates between estimating the cardiac bioelectric source across all heartbeats and then estimating cardiac positions for each heartbeat. We demonstrate that our geometric correction method is able to reduce geometric error and improve ECGI accuracy in a wide range of testing scenarios. We examine the performance of our geometric correction method using different activation sequences, ranges of cardiac motion, and body surface electrode configurations. We find that after geometric correction resulting ECGI solution accuracy is improved and variability of the ECGI solutions between heartbeats is substantially reduced. |
  Translational computer science at the scientific computing and imaging institute C. R. Johnson. In Journal of Computational Science, Vol. 52, pp. 101217. 2021. ISSN: 1877-7503 DOI: https://doi.org/10.1016/j.jocs.2020.101217 The Scientific Computing and Imaging (SCI) Institute at the University of Utah evolved from the SCI research group, started in 1994 by Professors Chris Johnson and Rob MacLeod. Over time, research centers funded by the National Institutes of Health, Department of Energy, and State of Utah significantly spurred growth, and SCI became a permanent interdisciplinary research institute in 2000. The SCI Institute is now home to more than 150 faculty, students, and staff. The history of the SCI Institute is underpinned by a culture of multidisciplinary, collaborative research, which led to its emergence as an internationally recognized leader in the development and use of visualization, scientific computing, and image analysis research to solve important problems in a broad range of domains in biomedicine, science, and engineering. A particular hallmark of SCI Institute research is the creation of open source software systems, including the SCIRun scientific problem-solving environment, Seg3D, ImageVis3D, Uintah, ViSUS, Nektar++, VisTrails, FluoRender, and FEBio. At this point, the SCI Institute has made more than 50 software packages broadly available to the scientific community under open-source licensing and supports them through web pages, documentation, and user groups. While the vast majority of academic research software is written and maintained by graduate students, the SCI Institute employs several professional software developers to help create, maintain, and document robust, tested, well-engineered open source software. The story of how and why we worked, and often struggled, to make professional software engineers an integral part of an academic research institute is crucial to the larger story of the SCI Institute’s success in translational computer science (TCS). |
  Prediction of Femoral Head Coverage from Articulated Statistical Shape Models of Patients with Developmental Dysplasia of the Hip P. R. Atkins, P. Agrawal, J. D. Mozingo, K. Uemura, K. Tokunaga, C. L. Peters, S. Y. Elhabian, R. T. Whitaker, A. E. Anderson. In Journal of Orthopaedic Research, Wiley, 2021. DOI: 10.1002/jor.25227 Developmental dysplasia of the hip (DDH) is commonly described as reduced femoral head coverage due to anterolateral acetabular deficiency. Although reduced coverage is the defining trait of DDH, more subtle and localized anatomic features of the joint are also thought to contribute to symptom development and degeneration. These features are challenging to identify using conventional approaches. Herein, we assessed the morphology of the full femur and hemi-pelvis using an articulated statistical shape model (SSM). The model determined the morphological and pose-based variations associated with DDH in a population of Japanese females and established which of these variations predict coverage. Computed tomography images of 83 hips from 47 patients were segmented for input into a correspondence-based SSM. The dominant modes of variation in the model initially represented scale and pose. After removal of these factors through individual bone alignment, femoral version and neck-shaft angle, pelvic curvature, and acetabular version dominated the observed variation. Femoral head oblateness and prominence of the acetabular rim and various muscle attachment sites of the femur and hemi-pelvis were found to predict 3D CT-based coverage measurements (R2=0.5-0.7 for the full bones, R2=0.9 for the joint). |
  Combining endocardial mapping and electrocardiographic imaging (ECGI) for improving PVC localization: A feasibility study W. W. Good, B. Zenger, J. A. Bergquist, L. C. Rupp, K. Gillett, N. Angel, D. Chou, G. Plank, R. S. MacLeod. In Journal of Electrocardiology, 2021. ISSN: 0022-0736 DOI: https://doi.org/10.1016/j.jelectrocard.2021.08.013 Introduction Objective
To implement and validate a combined epicardial/endocardial intramural activation time reconstruction technique. Methods
We used 11 simulations of ventricular activation paced from sites throughout myocardial wall and extracted endocardial and epicardial activation maps at approximate clinical resolution. From these maps, we interpolated the activation times through the myocardium using thin-plate-spline radial basis functions. We evaluated activation time reconstruction accuracy using root-mean-squared error (RMSE) of activation times and the percent of nodes within 1 ms of the ground truth. Results
Reconstructed intramural activation times showed an RMSE and percentage of nodes within 1 ms of the ground truth simulations of 3 ms and 70%, respectively. In the worst case, the RMSE and percentage of nodes were 4 ms and 60%, respectively. Conclusion We showed that a simple, yet effective combination of clinical endocardial and epicardial activation maps can accurately reconstruct intramural wavefronts. Furthermore, we showed that this approach provided robust reconstructions across multiple intramural stimulation sites. |